Information
Transforaminal epidural steroid injections (TFESI), also referred to as transforaminal nerve root injections or nerve root blocks, play a crucial role in both diagnosing and treating radicular pain. Distinguishing themselves from selective nerve root blocks (SNRB), TFESI primarily focuses on achieving an "epidural spill," ensuring the injectate reaches the epidural space. Although TFESI may be considered less selective than SNRBs, they offer valuable diagnostic insights and therapeutic benefits.
Indications:
Discogenic Radicular Pain:
TFESI is frequently employed in the diagnosis and management of discogenic radicular pain. This refers to pain originating from intervertebral discs that may be impinging on nerve roots, causing discomfort and radiating pain along the nerve pathways.
Painful Central Canal Stenosis (Lumbar):
The procedure is indicated for cases of painful central canal stenosis, particularly in the lumbar region. Central canal stenosis involves the narrowing of the spinal canal, leading to compression of the spinal cord or nerve roots, resulting in pain and other neurological symptoms.
Failed Back Syndrome:
TFESI is an effective intervention for individuals experiencing failed back syndrome. This condition, often characterized by persistent or recurrent pain following spinal surgery, can find relief through TFESI, addressing residual or new-onset radicular pain.
Non-Specific Low Back Pain:
TFESI is also utilized in the management of non-specific low back pain. While the causes of such pain may not be precisely identified, TFESI can provide therapeutic benefits by reducing inflammation and alleviating pain associated with the epidural space.
In conclusion, transforaminal epidural steroid injections are versatile procedures with a range of applications, offering both diagnostic precision and therapeutic relief for various conditions associated with radicular pain and spinal issues.
How long do lumbar epidural injections last for back pain?
The duration of pain relief from lumbar epidural injections varies, with studies suggesting effectiveness for up to six months in many cases. Lumbar epidural steroid injections (ESIs) are particularly successful in providing temporary relief for conditions like radicular pain from a lumbar herniated disc or spinal stenosis. Research indicates significant improvement, with up to 70% reporting at least 50% relief at one to two months post-injection, and 40% still experiencing relief at 12 months.
It's essential to recognize that lumbar ESIs don't aim to cure back pain but rather to alleviate symptoms, allowing individuals to manage pain and engage in rehabilitation efforts. This temporary relief can be a valuable part of a comprehensive pain management plan. Healthcare providers may suggest additional injections or alternative interventions based on the patient's response and the underlying condition.
Benefits
Advantages of Lumbar Epidural Steroid Injections:
Temporary Pain Relief:
Lumbar epidural steroid injections offer the benefit of providing temporary relief from low back pain. This can be particularly valuable for individuals experiencing acute or chronic pain, allowing them a respite from discomfort and the opportunity to engage in other therapeutic interventions.
Facilitation of Rehabilitation Exercises:
By alleviating pain, these injections can enable individuals to actively participate in rehabilitation exercises. Physical therapy and targeted exercises are crucial components of treating the underlying causes of low back pain. The temporary pain relief afforded by epidural steroid injections can enhance the effectiveness of rehabilitation efforts.
Improved Quality of Life:
Effective pain relief can contribute to an overall improvement in the quality of life for individuals with lumbar issues. Reduced pain levels often lead to enhanced physical functioning, improved mood, and an increased ability to perform daily activities, ultimately promoting a better quality of life.
Alternative to More Invasive Procedures:
Lumbar epidural steroid injections may serve as an alternative to more invasive procedures, such as surgery, for managing pain. By offering a non-surgical option, these injections provide a valuable intervention that can be considered before resorting to more extensive and potentially riskier treatments. For some individuals, successful pain management with epidural injections may negate the need for surgical interventions.
Complications
Complications arising from spinal interventional procedures, with specific relevance to transforaminal epidural steroid injections (TFESI), encompass a range of outcomes:
Transient, Increased Pain:
Patients may experience a temporary exacerbation of pain following TFESI. However, this heightened pain typically resolves without the need for further intervention. It is considered a transient response to the procedure.
Spinal Cord Infarction:
A serious complication associated with TFESI involves the occurrence of spinal cord infarction. This risk is present with both particulate and non-particulate steroids. Mechanisms leading to spinal cord infarction may include vascular compromise, vasospasm, or dissection. Careful consideration of steroid selection and injection technique is crucial to mitigate this rare but severe complication.
Numbness or Weakness:
Local anesthetics used during TFESI can lead to temporary numbness or weakness in the affected area. In some instances, patients may also exhibit symptoms of Horner syndrome, characterized by ptosis, miosis, and anhidrosis. This is typically a transient side effect and resolves as the effects of the local anesthetic wear off.
It is imperative for healthcare providers performing TFESI to be vigilant in monitoring patients for any signs of complications during and after the procedure. Additionally, thorough pre-procedure assessments and adherence to established guidelines can help minimize the risk of adverse events. Informed consent discussions should include a comprehensive overview of potential complications, ensuring that patients are well-informed about the procedure and its associated risks.
Procedure
Pre-Procedure Evaluation
Before conducting a transforaminal epidural steroid injection (TFESI), a comprehensive pre-procedure evaluation is essential. The practitioner should thoroughly review past imaging studies to inform technique and equipment selection. Correlating the patient's history and examination with imaging findings ensures accurate identification of the targeted side, level, and the type of procedure (e.g., epidural vs selective).
Equipment
Nonparticulate steroids, such as dexamethasone, are generally preferred over particulate steroids (e.g., triamcinolone, betamethasone) as per the United States Food and Drug Administration guidelines. This preference aims to reduce the risk of vascular complications like spinal cord infarction. However, it's important to note that complications have been reported with both types of steroids, and neither has been conclusively proven to be safer than the other. The use of blunt-tip needles is recommended to further minimize the risk of vascular complications.
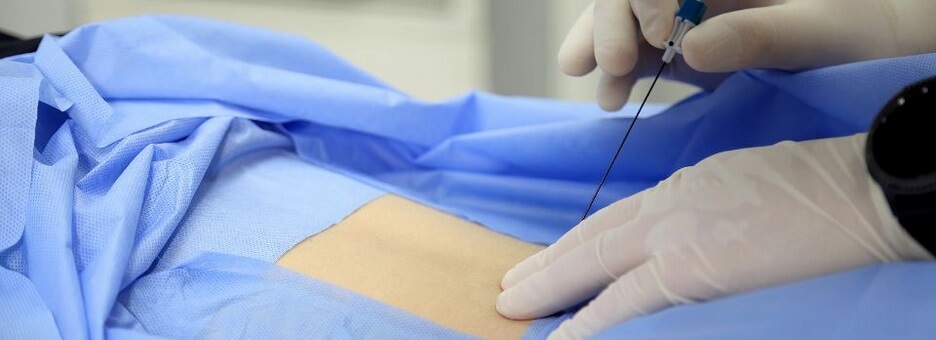
Technique
Fluoroscopy and CT are the primary imaging guidance methods for TFESI. The choice of technique depends on regional preferences, practitioner choice, equipment availability, and the type of injection. An infraneural approach (below the nerve root) is recommended to reduce the risk of vascular complications.
Under CT guidance, the needle can be advanced to the lumbar nerve root or into the epidural space. In cervical or thoracic injections, placing the needle tip on the lateral aspect of the facet joint is preferred to mitigate increased complication rates associated with intraforaminal injections. Despite this adjustment, good clinical outcomes are reported with indirect injections.
Contrast injection can be employed to exclude intravascular or intradural needle tip locations. However, the volume of contrast (e.g., 0.5-1 mL iodinated contrast media) and the pattern of contrast dispersion have not been shown to significantly impact clinical outcomes.
Upon achieving a satisfactory needle tip position, a mixture of anesthetic and/or steroids can be injected based on whether a diagnostic or diagnostic/therapeutic block is required. This step aims to provide pain relief and therapeutic effects in the targeted area.


