What is Microdiscectomy?
Microdiscectomy is a surgical procedure designed to alleviate pain and other symptoms caused by a herniated disc in the spine that is compressing the nerve root. During this operation, the surgeon aims to free the nerve by removing fragments of the herniated disc, bone, and ligament.
Microdiscectomy is often referred to as a minimally invasive spine surgery because it involves a small incision and the use of a microscope or surgical glasses, known as loupes, to magnify the surgical site. Additionally, smaller tools and instruments are utilized to work within the confined space of the spine. This procedure falls under the category of spinal decompression surgery, and the term "microdecompression" may also be used to describe the removal of any bone or ligament that compresses a nerve. However, "microdiscectomy" specifically pertains to the removal of the fragment of herniated disc tissue responsible for a patient's symptoms.
Microdiscectomy is typically recommended only after conservative treatments, such as physical therapy, steroid injections, and other medications, have been attempted for a period of at least 6 to 12 weeks without providing relief. In certain cases, motor weakness may prompt earlier surgery. Immediate surgical intervention is necessary for patients with cauda equina syndrome, a rare condition in which nerve pressure in the lower spine affects bladder and bowel function, but this condition affects less than 1% of individuals.
Lumbar microdiscectomy is a well-established and effective treatment for individuals suffering from the pain and discomfort associated with lumbar herniated discs. It is a preferred option when conservative treatments have proven ineffective in addressing the condition.
Microdiscectomy techniques include:
- Midline Microdiscectomy: In this technique, the surgeon makes a vertical incision, typically one to two inches in length, in the midline of the patient's back. The surgeon then lifts the surrounding muscles off the vertebrae and uses instruments to hold apart the layers of tissue during the procedure. While effective, this method may involve a bit more disruption to the surrounding tissues.
- Tubular Microdiscectomy: Tubular microdiscectomy is a minimally invasive approach in which the surgeon inserts a series of small tubes or dilators through a small incision. These tubes create a corridor through the muscle to reach the surgical site. This technique is designed to minimize disruption to the surrounding tissue and muscles, resulting in a faster recovery for the patient.
- Endoscopic Microdiscectomy: Endoscopic microdiscectomy, also known as microendoscopic discectomy, is an even more minimally invasive approach. In this technique, a smaller incision is made, and the surgeon uses a miniaturized camera and specialized instruments to perform the procedure. This method is associated with the least disruption to the surrounding tissues and muscles, providing for a quicker and less painful recovery for the patient.
The choice of microdiscectomy technique depends on various factors, including the patient's specific condition, the surgeon's expertise, and the desired balance between surgical effectiveness and minimal tissue disruption. All these techniques aim to remove the herniated disc material and relieve nerve compression with the least amount of surgical trauma possible.
Benefits
The benefits of a lumbar microdiscectomy procedure include:
- Pain Relief: The primary goal of microdiscectomy is to relieve pain and discomfort caused by a herniated disc compressing on a nerve root. By removing the disc fragment and any bone or ligament that is compressing the nerve, the surgery aims to alleviate pain.
- Minimally Invasive: Microdiscectomy is considered a minimally invasive procedure because it involves a small incision and uses specialized equipment, such as microscopes or surgical glasses, to magnify and access the surgical site. This results in less tissue damage and scarring.
- Precise Localization: Advanced imaging techniques, including X-rays, are used before and sometimes during the surgery to ensure accurate localization of the operative site. This precision helps the surgeon target the correct area and minimize the risk of damage to surrounding structures.
- Shorter Recovery Time: Microdiscectomy typically involves a quicker recovery compared to traditional open surgery. Many patients are able to return to their regular activities and work sooner.
- High Success Rate: Microdiscectomy is known for its high success rate in providing relief from pain and other symptoms associated with a herniated disc. It is a well-established and effective procedure.
- Conservative Approach: Before considering surgery, patients usually undergo conservative treatments such as physical therapy, steroid injections, and medication. Microdiscectomy is recommended when these treatments fail to provide relief, ensuring that surgery is pursued after non-invasive options have been exhausted.
- Lumbar Herniated Discs: While herniated discs can occur in various parts of the spine, microdiscectomy is most commonly performed in the lumbar (lower back) region, making it a well-practiced and successful procedure for this specific area.
The benefits of microdiscectomy make it an effective and favored treatment option for patients suffering from the pain and discomfort associated with herniated discs.
Procedure
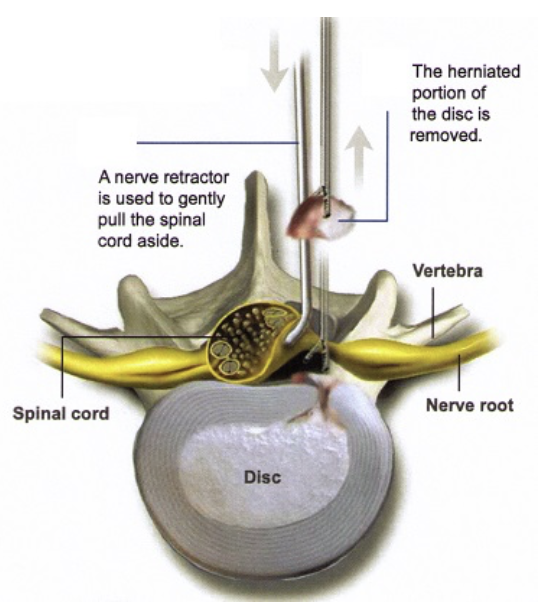
A microdiscectomy procedure aims to relieve nerve pressure by removing the disc material that is compressing the nerves. Here is an overview of the surgical process:
- Anesthesia: The procedure is performed under general anesthesia, so the patient is unconscious and cannot feel anything during the surgery.
- Patient Position: The patient is positioned prone for the surgery.
- Incision: A small incision, typically measuring 1 to 1 1/2 inches, is made directly over the affected disc.
- Microscope: A lighted microscope is used by the surgeon to provide a magnified view of the affected area, ensuring precise and accurate treatment.
- Bone Removal (if necessary): In some cases, the surgeon may need to remove a small portion of the bone that protects the nerve root to access the herniated disc.
- Herniated Tissue Removal: Using specialized instruments, the surgeon carefully removes the damaged herniated tissue, relieving the pressure on the nerve.
- Closure: The incision is closed with sutures.
- Recovery: Following the procedure, the patient is usually discharged on the same day or the next morning.
By removing the pressure on the nerve, the spinal nerve gains the necessary space within the spinal column, which should alleviate any pain caused by nerve compression. Microdiscectomy is known for its effectiveness in providing pain relief and improved nerve function for patients with herniated discs.
Lumbar Microdiscectomy procedure at Endospine360
If You Have Decided To Have Surgery:
- Call our doctors staff to schedule your surgery date and the date for your pre-operative consultation.
- At your pre-operative consultation doctor will discuss the procedure with you, answer any questions you may have, and have
- you sign a consent form for surgery.
- You will be given prescriptions for medicine and instructions for post-operative care.
- Your pre-operative evaluation will be scheduled on the same day as your pre-operative consultation. You may have a chest X-ray, ECG, ECHO & and blood-work performed.
- If you take aspirin or any blood thinner medications daily, STOP these medications at least 5 days before your surgery.
- If you are a smoker you should make every effort to stop smoking as soon as you can before surgery (at least 2 weeks prior to surgery). You should not smoke for at least 6 weeks after surgery.
Surgical Procedure:
- Your anesthesiologist will bring you to the operating room and put you to under anesthesia for the operation.
- A small incision (usually about one inch or less) is made in middle of your lower back
- After carefully moving the muscle tissue, a small retractor is placed to expose the back of the spine.
- A “window” to the spinal canal is created by removing a small amount of bone. This is called a laminotomy.
- The pinched nerve is gently moved to the side and the herniated disc material is removed from underneath the nerve. Only a small portion of disc material is removed.
- The incision is closed with resorbable stitches that are placed beneath the skin.
- The surgery will take approximately 1 hour.
After Surgery:
- You will be taken to the recovery room and stay there for about 1hour.
- Doctor will speak to your family while you are in the recovery room.
- The nurses will get you out of bed shortly after surgery and a physical therapist may work with you to ensure that you are strong enough to go home.
- You will be able to walk next day morning of surgery and usually discharged on post op day 2 of surgery.
After Going Home:
- A small dressing is placed over the incision in the operating room and remove this dressing 14 days after surgery.
- You will be given pain medication and a muscle relaxant to help control post-operative pain and spasms. Make sure you do not drive or operate heavy machinery while on the medication.
- There will be some activity restrictions that you will need to follow. For the first six weeks, no significant bending or twisting at the waist, and no lifting more than 20 lbs.
- You may drive once you are off of your medications (generally at about 10-15 days).
- You can expect to return to sedentary office or desk work approximately 10-15 days after surgery as long as you can maintain the activity restrictions.
- If you perform manual labor that requires heavy lifting or frequent bending or climbing, you should wait 6 weeks before returning to this activity.
- Sports activities such as badminton, Cricket or tennis may be resumed at 12 weeks.


