Information
Anterior Cervical Discectomy and Fusion (ACDF) is a surgical procedure performed in the neck region to address issues like herniated or degenerative discs that are causing neck or arm pain due to pinched nerves.
ACDF surgery is considered when conservative treatments like physical therapy and medications do not effectively relieve neck or arm pain caused by issues in the cervical spine. The procedure is typically performed on an outpatient basis, meaning patients can often go home on the same day as the surgery. Recovery and rehabilitation may vary depending on the individual patient and the specifics of the procedure. It's essential to follow post-operative care instructions and work closely with healthcare professionals to ensure a successful recovery.
ACDF surgery aims to alleviate pain and discomfort associated with cervical disc issues and prevent further problems caused by nerve compression. However, it may lead to some loss of range of motion, particularly if multiple levels are fused. The extent of range of motion loss varies based on neck mobility before surgery and the number of levels fused.
In some cases, artificial disc replacement may be an alternative to fusion. Artificial discs can preserve motion in the affected area, although their suitability depends on the individual's condition. Patients should discuss with their surgeon which approach, ACDF or artificial disc replacement, is most appropriate for their situation.
Types
Here are some common types of Anterior Cervical Discectomy and Fusion (ACDF):
- Single-Level ACDF: This is the most common type of ACDF and involves the removal of one cervical disc and the fusion of two adjacent vertebrae. It is typically used to address conditions such as a single-level herniated disc or cervical spondylosis.
- Two-Level ACDF: In a two-level ACDF, two cervical discs are removed, and the intervening vertebrae are fused together. This is used when two adjacent discs are causing symptoms or when degeneration occurs at two levels in the cervical spine.
- Three-Level ACDF: Three-level ACDF involves the removal of three cervical discs and the fusion of the corresponding vertebrae. This is a more extensive procedure and is used when three adjacent discs are causing symptoms or when degeneration occurs at multiple levels in the cervical spine.
- Cervical Corpectomy with ACDF: In cases where the damaged disc material is extensive, a cervical corpectomy may be performed. This involves the removal of both the disc and a portion of the vertebral body (corpus) that surrounds the disc. An ACDF is then performed to stabilize the spine after the corpectomy.
- Cervical Disc Replacement (Cervical Arthroplasty): While ACDF involves fusion, cervical disc replacement is an alternative technique that involves replacing the damaged disc with an artificial disc. This maintains motion at the treated level rather than fusing the vertebrae. It may be considered in select cases.
- Zero-Profile ACDF (Zero-P): In zero-profile ACDF, a small plate or spacer is used to replace the traditional plate and screws often associated with ACDF. This reduces the risk of post-operative complications associated with hardware and offers some advantages in specific cases.
- Minimally Invasive ACDF: Minimally invasive techniques use smaller incisions and less tissue disruption to access the cervical spine. These procedures aim to reduce post-operative pain and speed up recovery. The specific approach and instruments used can vary.
The choice of the type of ACDF procedure depends on the patient's diagnosis, the number of affected cervical discs, the extent of degeneration or damage, and the surgeon's judgment regarding the most appropriate surgical approach. Each type of ACDF has its own set of advantages and considerations, and the decision should be made in consultation with a spine specialist based on the individual patient's condition and needs.
Benefits
The Anterior Cervical Discectomy & Fusion (ACDF) approach offers several benefits, making it a preferred choice for many spine surgeons and patients:
Direct Access to the Disc: The anterior approach provides direct visualization and access to the cervical discs that are typically responsible for symptoms such as spinal cord or nerve compression. Removing these discs allows for direct decompression of the nerves and spinal cord. This approach can address a wide range of cervical spine levels, from the C2 segment down to the cervicothoracic junction (C7-T1), which is where the cervical spine joins with the upper spine (thoracic spine).
Less Postoperative Pain: ACDF is favored by many spine surgeons because it involves a relatively straightforward pathway to access the spine. Only one thin vestigial muscle needs to be cut, after which anatomical planes lead directly to the spine. The minimal muscle division or dissection results in less postoperative pain for patients. This is an advantage that contributes to a more comfortable recovery.
These advantages make the ACDF approach an attractive option for patients requiring cervical spine surgery, especially when addressing issues like spinal cord or nerve compression. However, it's important to note that the choice of surgical approach should be based on an individual's specific condition, the location of the affected discs, and other relevant factors. Your surgeon will evaluate your case and recommend the most suitable approach for your needs.
Here's an overview of the procedure:
These are essential steps to follow when preparing for surgery, as they help ensure a safe and successful procedure. It's important to adhere to your healthcare provider's recommendations and instructions before surgery. Here's a brief summary of the key steps:
- Disc Damage: The procedure is typically considered when there is damage to the cervical discs, which are the flexible cushions between the vertebrae in the neck. This damage, often due to wear and tear, can lead to issues like herniation or thinning of the discs, which may pinch the nearby nerves.
- Incision: The surgery is performed through an anterior approach, meaning the surgeon accesses the cervical spine from the front of the neck, specifically through the throat area. This approach allows for easier access to the cervical discs without disturbing the spinal cord, spinal nerves, and the strong neck muscles in the back.
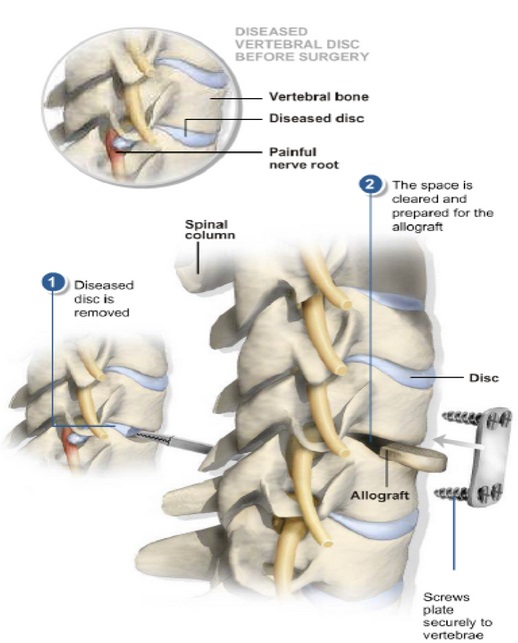
- Disc Removal: After making an incision, the surgeon carefully moves aside the neck muscles, trachea, and esophagus to expose the damaged disc and the bony vertebrae. The surgeon then removes the problematic disc.
- Spacer Bone Graft: After disc removal, there is an empty space between the bony vertebrae. To prevent the vertebrae from collapsing and rubbing together, a spacer bone graft is inserted to fill the open disc space. This bone graft acts as a bridge between the two adjacent vertebrae and promotes spinal fusion.
- Metal Plates and Screws: The bone graft and the vertebrae are secured in place using metal plates and screws. This hardware ensures stability and helps in the fusion process.
- Natural Healing Process: Following surgery, the body's natural healing process begins, and new bone cells start to grow around the bone graft. Over time, typically within 3 to 6 months, the bone graft fuses the two vertebrae, creating a single solid piece of bone. This fusion is similar to how reinforced concrete works, providing stability.
After Surgery:
Following an Anterior Cervical Discectomy & Fusion (ACDF) surgery, here's what you can expect in terms of the recovery process:
- Recovery Room: After the surgery, you will be taken to the recovery room, where you will stay for approximately 1 hour. This is the immediate post-operative phase where your vital signs and overall condition will be closely monitored.
- Transfer to Room: After your time in the recovery room, you will be transferred to your hospital room where you can have visitors, including your family.
- Length of Hospital Stay: You can typically expect to be discharged from the hospital around 2 days after the surgery. The specific length of your hospital stay may vary depending on your condition and the recommendations of your medical team.
- Family Consultation: Your doctor will speak to your family while you are in the recovery room to provide updates and discuss the procedure.
- Early Mobilization: Shortly after surgery, nurses and physical therapists will assist you in getting out of bed. Early mobilization is important for your recovery and helps prevent complications associated with prolonged bed rest.
- Dressing Change and Drain Removal: The surgical dressing will be changed the morning after surgery, and any small drainage tube that was placed may be removed. The new dressing will stay on for approximately 14 days, and your medical team will provide guidance on wound care during this period.
Recovery from ACDF surgery can vary from person to person. You may experience some post-operative discomfort or pain, and your medical team will provide pain management options. It's essential to follow their instructions for a smooth and successful recovery.
Keep in mind that the recovery process continues at home, and your surgeon will provide guidance on activity restrictions, pain management, and follow-up appointments as you transition to the next phase of your rehabilitation.
After Going Home:
- Pain Medication: You will be prescribed pain medication and a muscle relaxant to help manage post-operative pain and muscle spasms. Follow your doctor's instructions regarding medication use.
- Driving and Heavy Machinery: While taking pain medication, avoid driving or operating heavy machinery, as these medications can affect your alertness and coordination.
- Post-Operative Office Visit: You will have a post-operative office visit with your doctor approximately 2 weeks after surgery. During this visit, your surgeon will assess your progress and address any concerns you may have.
- Cervical Collar: You will need to wear a soft cervical collar continuously for the first 2 weeks after surgery. The collar provides support and immobilization to the neck during the initial healing period.
- Driving: You may resume driving after two weeks once you are out of the cervical collar and no longer taking medications that affect your ability to drive safely.
- Return to Work: If you have a sedentary office or desk job, you can typically expect to return to work approximately 1-2 weeks after surgery. Your specific return-to-work date may vary based on your individual progress.
- Manual Labor: If your job involves heavy lifting, frequent bending, or climbing, it's recommended to wait at least 3 months before returning to this activity. You can gradually transition back to moderate-duty work at 4-6 weeks.
- Follow-Up Appointments: You will see your doctor again 3 months after surgery for a follow-up evaluation.
- Rehabilitation Program: A rehabilitation program with a physical therapist will typically begin 6-12 weeks after surgery. This program is designed to help you regain strength and mobility in your neck.
- X-Rays: X-rays will be taken at each of your post-operative visits. The fusion of the cervical vertebrae is usually seen to be solid by 3 to 6 months.
- Resuming Sports Activities: If the fusion is solid, you may resume sports activities such as golf or tennis at 3 months post-surgery. The timing for returning to sports should be discussed with your doctor and based on your individual progress.
It's essential to follow your surgeon's recommendations and guidelines for a successful recovery. Your surgeon and medical team will provide you with specific instructions tailored to your condition and progress.