Information
Interlaminar Endoscopic Spine Surgery is a specific form of endoscopic surgery that utilizes an interlaminar approach. The choice between the transforaminal or interlaminar endoscopic approach is determined by the type of pathology or condition affecting the patient.
This approach typically involves accessing the spine through a small incision between adjacent laminae. It is a technique employed based on the specific needs and diagnosis of the patient.
The flexibility of the interlaminar endoscopic technique makes it a versatile option for dealing with various pathologies. When it comes to surgical treatment for high-grade migrated disc herniation, patients who undergo Transforaminal Endoscopic Lumbar Discectomy (TELD) for severely migrated discs tend to experience less favorable clinical and radiological outcomes compared to those with near-migrated discs. In such cases, open surgery should be considered.
Transforaminal Endoscopic Lumbar Discectomy (TELD) involves foraminoplasty, which entails partial removal of the ventral facet and/or pedicle to increase the width of the foramen and access the anterior epidural space. In contrast, Interlaminar Endoscopic Lumbar Discectomy (IELD) can reach far-migrated disc fragments without the need for facet joint or pedicle damage, which could lead to subsequent instability.
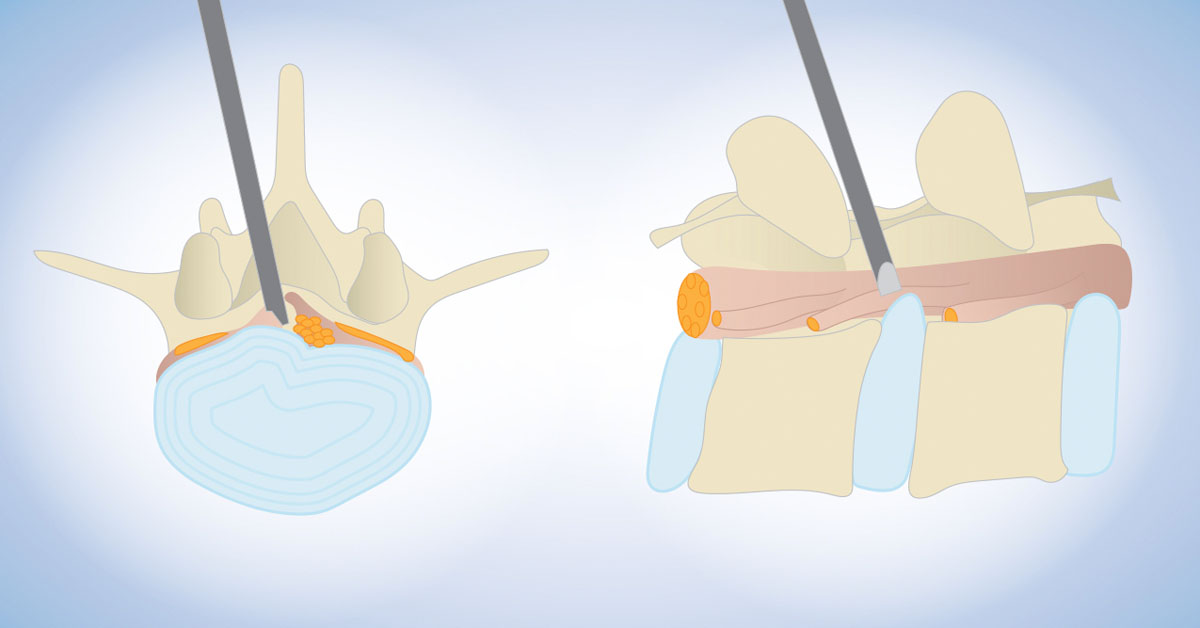
Through the interlaminar window, the cranio-caudal trajectory of the endoscope is flexible and can be tailored based on the pre-operative evaluation of the migrated fragment. For selected patients with high-grade inferior-migrated L4–5 disc herniation, L5–S1 IELD can remove sequestrated disc material through a wide interlaminar window without the need for bony destruction. In cases where there is an overhang lamina, surgeons can employ customized laminotomy techniques to widen the interlaminar window and use endoscopes of different sizes to access far-migrated disc fragments. This approach provides a versatile and effective option for addressing challenging disc herniations.
Types of Interlaminar endoscopic techniques include:
- Interlaminar Endoscopic Lumbar Discectomy (IELD): This procedure involves assessing and treating lumbar disc issues through the interlaminar approach, which allows for minimally invasive removal of herniated disc material.
- Percutaneous Stenoscopic Lumbar Decompression (PSLD): PSLD is a minimally invasive approach to alleviate lumbar spinal stenosis. It involves the use of a stenoscope to perform decompression procedures while preserving spinal stability.
- Lumbar Endoscopic Unilateral Laminotomy for Bilateral Decompression (LE-ULBD): This technique involves a unilateral laminotomy, which is the removal of a portion of one lamina, to perform decompression on both sides of the spine. It allows for the treatment of conditions such as spinal stenosis and herniated discs.
These interlaminar endoscopic techniques offer less invasive alternatives to traditional open surgeries for various spinal conditions, providing patients with the benefits of reduced tissue damage, shorter recovery times, and smaller incisions.
Benefits
The interlaminar endoscopic technique offers several benefits for patients undergoing spine surgery. Some of these advantages include:
- Minimally Invasive: Interlaminar endoscopic surgery involves small incisions, resulting in less tissue damage and scarring compared to traditional open surgery.
- Reduced Postoperative Pain: Patients often experience less pain after interlaminar endoscopic surgery, which may lead to decreased reliance on pain medications.
- Shorter Hospital Stay: The minimally invasive nature of these procedures typically allows for shorter hospital stays and quicker recovery times.
- Faster Return to Normal Activities: Patients can often return to their regular activities sooner, reducing disruption to their daily lives.
- Preservation of Spinal Stability: These techniques aim to preserve spinal stability, reducing the risk of subsequent instability or complications.
- Customized Approaches: The interlaminar technique can be tailored to the patient's specific condition, providing versatile treatment options.
- Less Risk of Postoperative Infection: Smaller incisions and less tissue disruption are associated with a decreased risk of postoperative infections.
- Targeted Treatment: These techniques allow for precise targeting of the affected area, resulting in more effective treatment.
- Reduced Scarring: The minimal tissue disruption and smaller incisions lead to less noticeable scarring, which is particularly important for cosmetic and comfort reasons.
- Versatile Application: Interlaminar endoscopic techniques can be used to address a wide range of spinal conditions, making them suitable for various patients and diagnoses.
These benefits make interlaminar endoscopic techniques an appealing option for many individuals seeking relief from spinal conditions while minimizing the impact on their daily lives and overall well-being.
Procedure
The procedure for interlaminar endoscopic spine surgery involves several steps:
- Patient Preparation: Before the surgery, the patient will undergo a thorough evaluation, including a review of medical history and imaging studies (e.g., MRI or CT scans) to precisely identify the source of the spinal problem.
- Anesthesia: The patient is typically given local or epidural anesthesia for surgery will take place. This allows the patient to remain awake and aware during the procedure while ensuring comfort.
- Incision: A small incision is made. The size of the incision is minimal, typically about the diameter of a pencil (5-8 mm).
- Endoscope Insertion: An endoscope, a thin, flexible tube with a camera and light source, is inserted through the small incision. This provides real-time visualization of the surgical site.
- Tissue Retraction: Soft tissues, such as muscles and ligaments, are gently retracted to access the laminae, which are the part of bone that form the spinal canal.
- Decompression: Depending on the patient's specific condition, decompression procedures are performed. This may include removing herniated disc material, bone spurs, or other sources of compression on nerves.
- Closure: Once the surgical objectives are achieved, the endoscope is removed, and the incision is closed with sutures or adhesive strips. The minimal size of the incision results in less noticeable scarring.
- Recovery: After the surgery, the patient is encouraged to walk and move around to assess immediate pain relief. Patients can usually have a meal and are often required to stay in the hospital for a short period, typically overnight.
- Follow-up: Patients are scheduled for a follow-up appointment, typically within 2 weeks, to monitor their progress and ensure proper healing. Depending on the patient's specific condition, the doctor may recommend physical therapy or rehabilitation.
The specific steps of the procedure may vary depending on the patient's diagnosis and the surgeon's approach. Interlaminar endoscopic techniques offer the advantage of minimal tissue disruption, faster recovery, and reduced postoperative pain compared to traditional open surgeries.


