What is Laminectomy?
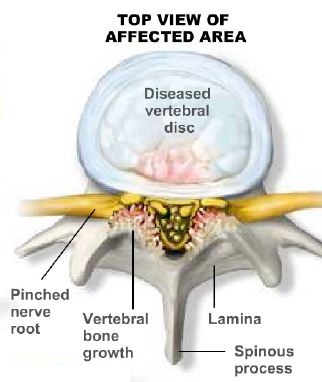
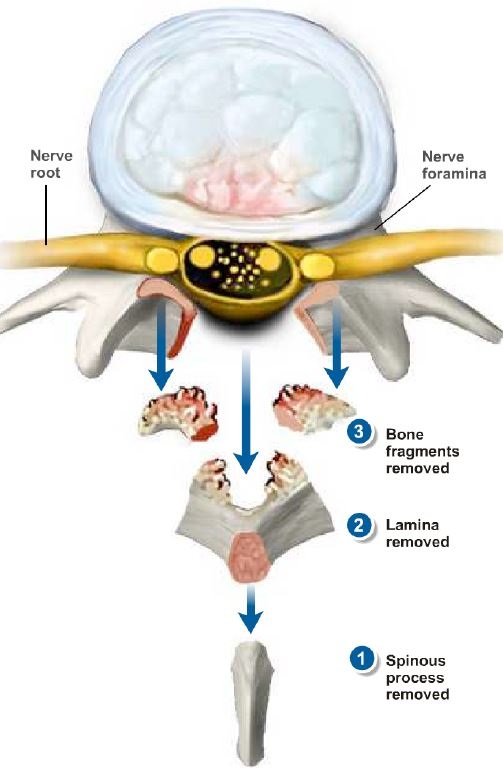
Laminectomy is a surgical procedure designed to create space within the spinal canal by removing bone spurs and associated tissues that are often linked to spinal arthritis. This procedure typically involves the removal of a small portion of the back part (lamina) of the vertebral bones, which make up the spine. The primary goal of laminectomy is to enlarge the spinal canal, thus alleviating pressure on the spinal cord or nerves. It is commonly performed as part of a decompression surgery.
The pressure on the spinal cord or nerves that necessitates a laminectomy is frequently caused by the presence of bony overgrowths within the spinal canal, which can develop in individuals with spinal arthritis. These overgrowths are often referred to as bone spurs and are a natural result of the aging process for some people. In some cases, bone spurs may also have a hereditary component.
Laminectomy is typically considered when less invasive treatments, such as medication, physical therapy, or injections, have not effectively relieved the symptoms. It may also be recommended when symptoms are severe or rapidly worsening. This surgical procedure is intended to address the underlying cause of spinal compression and provide relief to patients who are experiencing pain and other neurological symptoms.
A healthcare provider may recommend a laminectomy in the following situations:
Failure of Conservative Treatment: When conservative treatments, like medication or physical therapy, do not effectively improve the patient's symptoms, a laminectomy may be considered as the next step in managing the condition.
Muscle Weakness or Numbness: If the patient experiences muscle weakness or numbness that significantly impairs their ability to stand or walk, a laminectomy may be recommended to address the underlying spinal issue causing these symptoms.
Loss of Bowel or Bladder Control: When symptoms include a loss of bowel or bladder control, which could indicate a serious issue with spinal compression, a laminectomy may be required to relieve the pressure on the spinal cord or nerves.
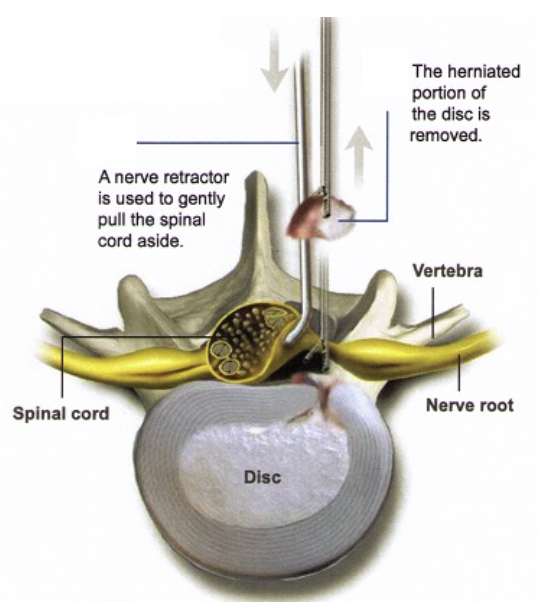
In some cases, a laminectomy may also be performed as part of surgery to treat a herniated spinal disk. The surgeon may need to remove a portion of the lamina to access and address the damaged disk, thereby relieving nerve compression and related symptoms.
Lumbar laminectomy is a surgical procedure that involves the removal of the lamina, a bony arch on the back of a lumbar (lower) vertebra, to create more space within the spinal canal. This procedure is commonly performed to relieve pressure on the spinal cord or nerves in the lumbar spine, particularly for conditions such as lumbar spinal stenosis, herniated discs, and other causes of nerve compression. There are different types of lumbar laminectomy procedures, depending on the extent of removal and the specific approach used.
Here are some common types of lumbar laminectomy:
- Partial Laminectomy: In a partial laminectomy, only a portion of the lamina is removed to create more space in the spinal canal while leaving the remainder of the lamina intact. This approach is often used when decompression is needed but preserving spinal stability is a concern.
- Complete Laminectomy: A complete laminectomy involves the full removal of the entire lamina, providing maximum space for spinal cord or nerve decompression. This approach may be necessary for severe cases of spinal stenosis or other conditions where a substantial amount of space is required.
- Bilateral Laminectomy: Bilateral laminectomy refers to the removal of the lamina on both sides of the spine. This procedure is used when nerve compression occurs on both sides of the spinal canal. It is often performed in cases of central spinal stenosis or bilateral disc herniations.
- Unilateral Laminectomy: Unilateral laminectomy involves the removal of the lamina on only one side of the spine. It is typically performed when the spinal problem is localized to one side, and the goal is to create more space for nerve decompression without disturbing the other side of the spine.
- Laminectomy with Fusion: In some cases, a laminectomy may be combined with spinal fusion. Fusion involves the use of bone grafts or spinal instrumentation (such as screws and rods) to stabilize the spine after the lamina is removed. This procedure is typically used when there are concerns about spinal instability.
- Minimally Invasive Laminectomy: Minimally invasive techniques aim to achieve the goals of laminectomy with smaller incisions and less tissue disruption. These techniques use specialized tools and endoscopic approaches to access the lamina and perform the decompression, resulting in reduced post-operative pain and faster recovery.
The specific type of lumbar laminectomy performed depends on the patient's diagnosis, the location of the spinal problem, the extent of nerve compression, and the surgeon's assessment of the most appropriate approach to relieve symptoms and improve spinal function. Patients should consult with a spine specialist to determine the best surgical approach for their individual condition and discuss the potential risks and benefits of each type of laminectomy procedure.
Benefits
Lumbar laminectomy offers several benefits, including:
- Small Incision: The incision made for a lumbar laminectomy is typically one inch or even smaller. This minimally invasive approach results in less tissue disruption and a smaller scar.
- Minimal Blood Loss: Due to the small incision and precise surgical technique, lumbar laminectomy is associated with minimal blood loss during the procedure.
- Quick Recovery: Many patients who undergo lumbar laminectomy experience a relatively quick recovery. They can often return to work within days and resume sports or other physical activities in approximately six weeks. This faster recovery timeline is attributed to the minimally invasive nature of the procedure.
Lumbar laminectomy is an effective surgical option for individuals with specific spinal conditions, and these advantages make it an attractive choice for those seeking relief from symptoms related to spinal compression.
The surgical procedure for a lumbar laminectomy typically follows these steps:
- Anesthesia: Your anesthesiologist will administer anesthesia to put you to sleep for the operation.
- Operating Room Setup: The operating room will have a team, including two nurses and a surgical assistant, to support the doctor during the procedure.
- Incision: An incision is made in the middle of your lower back, with the length of the incision determined by the number of spinal levels that need to be decompressed.
- Muscle Tissue Handling: After making the incision, the surgical team carefully moves the muscle tissue aside to access the back of the spine.
- Retractor Placement: A retractor is placed to further expose the spinal canal area, allowing the surgical team to work on the spine.
- Bone and Ligament Removal: Bone and ligaments that are causing pressure on the spinal canal are removed to create more space for the spinal cord and nerves.
- Discectomy (if required): If a discectomy is part of the procedure, the pinched nerve is gently moved aside, and the bulging or herniated disc material is removed from underneath the nerve.
- Closure: The incision is closed with resorbable stitches that are positioned beneath the skin.
The duration of the surgery may vary depending on the number of spinal levels involved, but it typically takes about one hour or more. The procedure is designed to alleviate pressure on the spinal cord or nerves, addressing symptoms related to spinal compression.
After the surgery
- You will be taken to the recovery room immediately after the surgery. Typically, patients stay in the recovery room for about 1 hour.
- The doctor will take this time to speak with your family and provide them with an update on your condition and the outcome of the procedure.
- The nursing staff will encourage you to get out of bed shortly after the surgery. This early mobility is essential for your recovery. In some cases, a physical therapist may work with you to assess your strength and ensure you are ready to go home.
- Patients can often walk in the morning following the surgery. It's a significant step in the recovery process.
- In many cases, patients are discharged from the hospital on the second day after the surgery, known as the post-operative day 2.
After Going Home:
Following your surgery, you can anticipate the following post-operative care and restrictions:
- The dressing over the incision is typically removed 14 days after the surgery.
- You will be provided with pain medication and a muscle relaxant to manage post-operative pain and muscle spasms. During this time, it's essential not to drive or operate heavy machinery while taking these medications.
- There will be specific activity restrictions during your recovery. For the first six weeks, avoid significant bending or twisting at the waist, and refrain from lifting anything over 20 lbs.
- You may resume driving once you are off the medications, generally around 10-15 days post-surgery.
- Sedentary office or desk work can typically be resumed about 10-15 days after surgery, as long as you can maintain the activity restrictions.
- If your work involves manual labor with heavy lifting, frequent bending, or climbing, it's advisable to wait for 6 weeks before returning to such activities.
- Sports activities like badminton, cricket, or tennis may be resumed at approximately 12 weeks post-surgery.
It's crucial to follow your medical team's guidance regarding these restrictions to ensure a successful recovery and minimize the risk of complications. Your specific recovery plan may be adjusted based on your progress and individual circumstances.


