- Home
- Understanding the Risks of Spine Surgery

- Home
- Understandi...
Understanding the Risks of Spine Surgery
There are many potential complications that can occur with spine surgery, and listing them one-by-one can be a bit overwhelming. It is easier to break the risks into categories to help making understanding them easier.
There are three general categories of risk with any surgery, including spine surgery:
- Complications related to Anesthesia
- Complications related to surgery- Intra-operative & Post-operative
- Medical complications
RISKS OF ANESTHESIA
Most spinal operations require general anesthesia. Although all types of anesthesia involve some risk, major side effects and complications from anesthesia are uncommon. Your specific risks depend on your health, the type of anesthesia used, and your response to anesthesia.
These risks can include:
- Allergic reaction to medications
- Nausea and vomiting after the surgery
- Hoarseness of the voice
- Damage to the teeth or lips
- Soreness/swelling of the throat
- Changes in blood pressure
- Changes in heart rate or rhythm
- Heart attack
- Stroke
- Death – risk is 1 out of 200,000
RISKS OF COMPLICATIONS DURING THE SURGERY (INTRAOPERATIVE)
- Dural tear and spinal fluid leak – 1%
- Nerve or spinal cord injury – 1 out of 5,000
- Abnormal bleeding
- Injury to nearby anatomical structures – rare
Nerve or Spinal Cord Injury
Any time surgery is done on the spine, there is some risk of injuring the spinal cord or the individual nerves. This can occur from instruments used during surgery, from swelling, or from scar formation after surgery. Damage to the spinal cord can cause paralysis in certain areas and not others. Injured nerves can cause pain, numbness, or weakness in the area supplied by the nerve. If a nerve is damaged that connects to the pelvic region, it may cause sexual dysfunction.
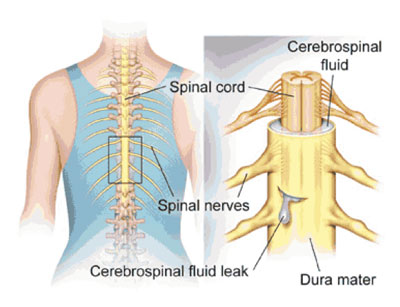
Dural Tear
Durameter is a water-tight sac of tissue that covers the spinal cord and the spinal nerves. It is not uncommon to have a dural tear during any type of spine surgery. If noticed during the surgery, and the tear is small it is just covered with muscle patch and heals on its own.If the tear is >5 mm the tear is simply repaired and usually heals uneventfully. Sealants like duragen patch and fibrin glue can be used as adjuvants.
If it is not recognized, the tear may not heal and may continue to leak spinal fluid, which can cause problems later. The leaking spinal fluid may cause a spinal headache. It can also increase the risk of infection of the spinal fluid (spinal meningitis).
(RISKS OF COMPLICATIONS AFTER THE SURGERY (POST-OPERATIVE)
- Wound Infection – 1%
- Dural tear and spinal fluid leak (see above – rarely, this can develop after surgery)
- Blood clots in the legs (DVT)
- Medical complications (heart attack, stroke, pneumonia, urinary infection)
- Implant & Fusion Complications
Infection
There is a risk of infection any time surgery is performed. Infections occur in 1-2% of spinal surgeries.
An infection can be in the skin incision only, or it can spread deeper to involve the areas around the spinal cord and the vertebrae. A superficial wound infection can usually be treated with antibiotics, and perhaps removing the skin stitches. The deeper wound infections can be very serious and will probably require additional operations to drain the infection. In the worst cases, any bone graft, metal screws, or plates that were used may need to be removed.
Persistent Numbness, Weakness or Burning
Immediately after surgery, it is not unusual for some of the same symptoms you experienced before surgery (numbness, weakness, burning) to continue. It sometimes takes a while for your nerves to recover, and in most cases these continuing symptoms will gradually resolve as you recover from your surgery.
Recurrence
In 2-5% of patients, re-herniation of disc can occur from the torned annulus. It is usually common in first 2-3 months of surgery but can also occur later if proper postural care and exercise protocol is not followed. In case of recurrence, surgical options can range from dissectomy again or fusion of the degenerated disc.
Implant & Fusion Complications
Cage or Bone Graft Migration
In some spine surgeries, a disc between the vertebrae may be removed and replaced with a fusion cage or structural piece of bone graft. Migration is a term used to describe a fusion cage or bone graft that has moved out of place. When this happens, it usually occurs soon after surgery, before the cage or graft is firmly attached by bone growth. If the cage or graft moves too far, it may not be doing its job of stabilizing the two vertebrae. If it moves backwards towards the spinal cord, or forward towards the structures in front of the spine, it may damage those structures. A problem with migration may require a second operation to replace the cage or graft that has moved.
Nonunion (Failed Fusion)
A certain number of fusions simply do not heal as planned. This failure of the fusion to heal is called a “nonunion”. A nonunion usually means that there is motion between the two bones that should be fused together. This unwanted motion can result in pain that may increase over time. The spinal motion can also stress the metal implants used to hold the fusion together, possibly causing the implants to break. You may need additional surgery for a nonunion to try to get the bones to fuse together. Your surgeon might want to add more bone graft, replace the metal hardware, or add an electrical stimulator to try to get the fusion to heal.
Hardware Loosening or Fracture
Metal screws, plates, and rods are used in many different types of spinal operations as part of the procedure to hold the vertebrae in alignment while the surgery heals. These metal devices are called “hardware”. Once the bone fusion heals, the fusion becomes more resistant to stress than the hardware. Sometimes the hardware can either loosen or break before the fusion is completely healed. If this occurs it may require a second operation to either remove or replace the hardware.
 DURAL TEAR
DURAL TEAR


