What is a Herniated Disc?
A herniated disc, also referred to as a prolapsed disc, occurs when the tough, outer fibers of the intervertebral disc become damaged, causing the inner soft material, known as the nucleus pulposus, to rupture out of its designated area.
This displaced disc material has the potential to encroach upon the spinal canal, exerting pressure on the spinal cord, although more commonly, it affects the spinal nerves.
It's worth noting that herniated discs are a relatively rare occurrence in children and are predominantly found in young and middle-aged adults. The development of a herniation can transpire suddenly or progress gradually over a period of several weeks or even months.
Herniated Disc:
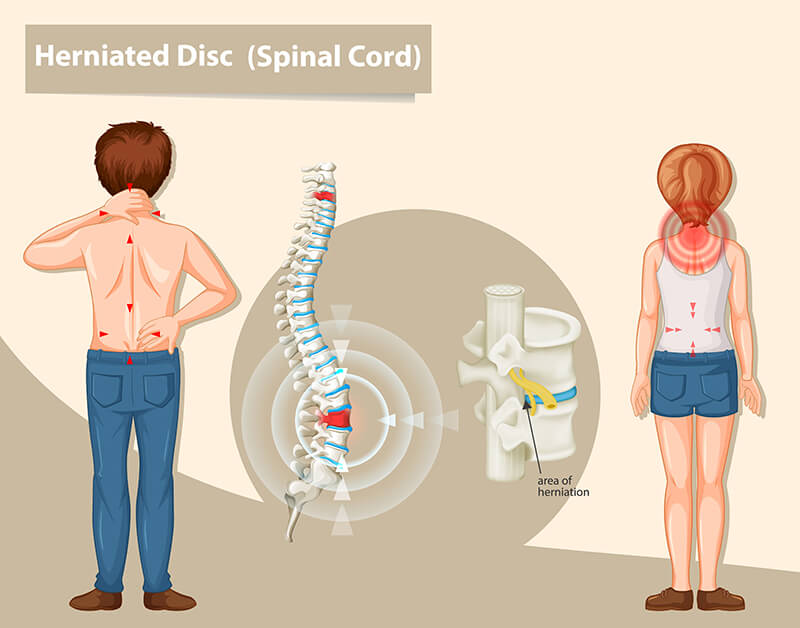
Herniated discs can manifest in any region of the spine. While they are more prevalent in the lower back, also known as the lumbar spine, they can also occur in the neck, which is referred to as the cervical spine. The specific location of pain and symptoms experienced largely depends on which segment of the spine is affected.
Symptoms
Symptoms of a herniated or prolapsed disc can vary among individuals, and not everyone experiences back or neck pain, although such pain is a common manifestation.
The primary symptoms of a herniated disc typically include:
- In severe cases, loss of bladder or bowel control, along with numbness in the genital area, and impotence in men.
- Numbness, a sensation of pins and needles, or tingling in one or both arms or legs.
- Pain localized behind the shoulder blade(s) or in the buttock(s).
- Radiating pain that travels down one or both arms or legs.
- Weakness affecting one or both arms or legs.
The specific location of these symptoms is determined by the nerves that have been affected, thereby aiding in the diagnosis process.
Causes
Intervertebral discs can experience sudden prolapse due to excessive pressure,and notable examples of such scenarios include:
- Falling from a significant height and landing on your buttocks, which can transmit a considerable force across the spine. In cases where the force is exceptionally strong, it can lead to either a fracture of a vertebra (bone) or a rupture of an intervertebral disc.
- Bending forward places substantial stress on intervertebral discs. When you bend and attempt to lift an object that exceeds your capacity, the force generated in this process may result in a disc rupture.
It's important to note that intervertebral discs can also rupture due to the gradual weakening of their outer fibers. This weakening typically occurs as a result of repeated minor injuries that accumulate over time. Factors such as aging, genetic predisposition, and activities related to work or recreation can contribute to this damage. Often, there may be no apparent reason for this process to occur.
However, at some point, a specific action like lifting a heavy object or making a twisting or bending movement can exert enough pressure on the disc, causing it to rupture through its weakened outer fibers.
Herniated Disc most frequently occur in two regions of the spine:
The lumbar spine (lower back) and the cervical spine (neck). They are less commonly found in the thoracic spine (mid-back region).
A Herniated disc can give rise to problems in two primary ways:
- Direct pressure: When the disc material ruptures into the spinal canal or intervertebral foramen, it can exert pressure on the nerves or the spinal cord.
- Chemical irritation: After a rupture, the core material of the disc can cause chemical irritation to the nerve roots, resulting in inflammation of the nerves.
Both the direct pressure on the nerve root and the chemical irritation can adversely affect the functioning of the nerve root, leading to various issues.
Diagnosis
Diagnosing a herniated disc typically initiates with a comprehensive history-taking by your specialist, often followed by a pertinent physical examination.
Your spine surgeon will focus on specific questions, including:
- History of Injury: Did you experience an injury before the onset of pain?
- Location of Pain: Where exactly is the pain localized?
- Numbness or Pins and Needles: Are you experiencing any sensations of numbness or pins and needles?
- Weakness: Is there any noticeable weakness?
- Prior Similar Issues: Have you encountered a similar problem before?
- Recent Health Changes: Have you undergone any recent changes such as weight loss, fevers, or other illnesses?
Additionally, your doctor or spine surgeon will inquire about any difficulties with walking, as well as any challenges related to bladder or bowel control. While these inquiries may seem unrelated, they are essential to ascertain whether there is significant pressure from the herniated disc on the spinal cord or nerves that could impact bowel and bladder function. Such symptoms may indicate an emergency, necessitating immediate investigation and, in some cases, surgery.
A definitive diagnosis is typically achieved through radiological investigations.
An MRI scan is considered the most accurate diagnostic tool; however, it's important to note that smaller prolapses may be missed, particularly since most of these scans are conducted with patients lying flat, which places less pressure on the disc and may show less bulging than when sitting.

Other investigations that your neurosurgeon or spinal surgeon may arrange include a CT myelogram (involving the injection of dye into the spinal canal followed by a CT scan) and a nerve sheath injection with a local anesthetic, which can help confirm the exact nerve responsible for your symptoms.
Treatment
In the majority of cases, around 80 to 90%, disc prolapses tend to resolve on their own, with symptoms gradually disappearing. This natural healing process typically unfolds over a span of 6 to 8 weeks, although it may extend beyond this timeframe.
In the absence of substantial evidence indicating significant compression of the spinal cord or nerve root or a noticeable impairment in function, acute disc prolapses are typically managed conservatively initially. This conservative approach frequently involves a combination of anti-inflammatory drugs and pain relief medications. In addition, a physiotherapy regimen is often recommended, and in some instances, hydrotherapy and pilates may be incorporated.
If symptoms persist and do not respond to conservative treatment, intervention may become necessary. This intervention can include a nerve block with a local anesthetic or surgical procedures. Studies have shown that surgery can expedite recovery following a disc prolapse.
The treatment provided to each individual is tailored to their unique clinical presentation, radiological findings, and other relevant factors. Your spine surgeon will craft a treatment plan specific to your situation, and this plan will be subject to periodic review and adjustments as needed.



