Spine TB
What Is Spinal Tuberculosis?
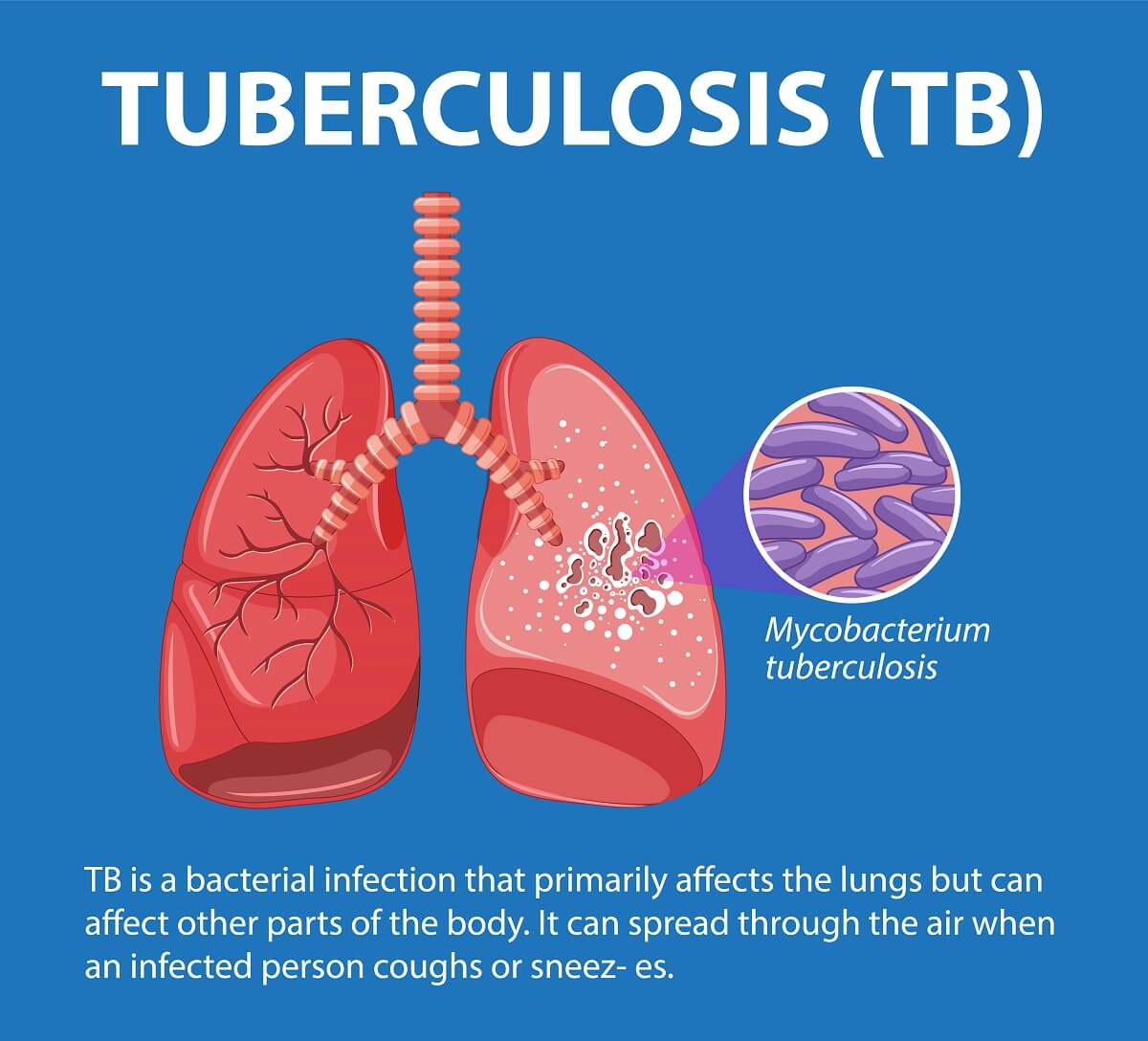
Tuberculosis (TB) is a serious bacterial infection that poses a significant threat if not properly treated. It is primarily caused by the bacterium Mycobacterium tuberculosis and commonly targets the lungs. However, it has the potential to affect various other organs and tissues, including bones. Spinal tuberculosis, known medically as Pott's disease, stands as the most prevalent form of TB impacting the skeletal system.
Stages of Bone Tuberculosis
Bone tuberculosis, including spinal tuberculosis, typically advances through several distinct stages:
- Synovitis: Initially, individuals may experience night pain and muscle spasms as the infection affects the bones.
- Early arthritis: As the disease progresses, joint pain intensifies along with muscle spasms, leading to some impairment in daily activities.
- Late arthritis: Pain and spasms become more pronounced, significantly reducing functionality. There may be a loss of over 75% of the joint's range of motion.
- Advanced arthritis with subluxation and dislocation: At this stage, deformities may develop in the affected joints, and there is a severe restriction in movement.
- Terminal arthritis: The joint becomes fused, losing its ability to move altogether.
Symptoms
Symptoms of Spinal Tuberculosis
Symptoms of spinal tuberculosis primarily affect the thoracic (upper back) and lumbar (lower back) regions of the spine. Initially, these symptoms can be subtle and nonspecific, but as the disease progresses, they can become more pronounced.
Early symptoms of spinal tuberculosis include:
- Back pain: Persistent discomfort in the affected area.
- Muscle spasms: Involuntary contractions of muscles surrounding the spine.
- Stiffness: Difficulty in moving the spine freely.
As spinal tuberculosis advances, additional symptoms may emerge, such as:
- Joint deformities/scoliosis: Abnormal curvature of the spine or deformities in the affected joints.
- Swelling: Inflammation and swelling around the affected area.
- Decreased range of motion: Limited ability to move the spine.
- Ulcers: Skin lesions or wounds that may develop due to the infection.
- Swollen lymph nodes: Enlargement of lymph nodes near the infected area.
- Cold abscess: Formation of pockets of pus in the affected region.
Moreover, spinal tuberculosis can exert pressure on the spinal cord and adjacent nerves, leading to neurological symptoms such as:
- Weakness in the legs: Reduced strength or difficulty in moving the lower limbs.
- Numbness and tingling: Sensory disturbances in the legs or other affected areas.
- Paralysis: Loss of motor function in severe cases.
It's important to note that not everyone with spinal tuberculosis will exhibit typical symptoms of tuberculosis. Only about one-third of individuals with bone tuberculosis, including spinal tuberculosis, may experience classic TB symptoms such as:
- Decreased appetite
- Low-grade fever (often occurring at night)
- Weight loss
- Chills
- Weakness
- Fatigue
These symptoms may vary in intensity and manifestation among individuals, underscoring the importance of early diagnosis and treatment for spinal tuberculosis.
Causes
Spinal tuberculosis, also known as Pott's disease, arises when the bacterium Mycobacterium tuberculosis infects the vertebrae, which are the bones that make up the spine. This bacterium is primarily transmitted through the air from person to person. While tuberculosis affecting the lungs is highly contagious, tuberculosis affecting other parts of the body, including the spine, is not typically as contagious. However, once the bacterium is transmitted from an infected individual to another, it can potentially spread from the lungs to other areas of the body, including the spine.
Diagnosis
Spinal tuberculosis, though not widespread, poses challenges in timely diagnosis due to its relatively low occurrence rate. It affects approximately 1% to 3% of individuals with tuberculosis (TB). Furthermore, diagnosing spinal TB is often delayed because its symptoms mimic those of more prevalent conditions like arthritis or muscle strain, which also manifest as back pain and stiffness.
One distinguishing factor is that individuals with spinal tuberculosis typically lack the lung infection commonly associated with tuberculosis. This absence of lung involvement in spinal TB cases further complicates diagnosis since healthcare providers may not initially consider TB as a potential cause of the symptoms.
Skin and Blood Tests
To detect the presence of Mycobacterium tuberculosis in the body, healthcare providers typically rely on skin or blood tests.
The Mantoux tuberculin skin test involves injecting a small amount of tuberculin-purified protein derivative under the skin, usually on the inner forearm. The test site is then examined 48 to 72 hours later. A positive result is indicated by the presence of a firm, swollen bump measuring 5 millimeters or more. This suggests recent exposure to someone with TB.
Blood tests are another method for detecting TB bacteria. However, it's important to note that neither skin nor blood tests specifically diagnose spinal tuberculosis; they merely indicate the presence of the bacteria in the body.
For a more accurate diagnosis of spinal tuberculosis, a tissue acid-fast bacilli culture test is ideal. However, obtaining a sample for this test can be challenging. Furthermore, the results often take six or more weeks to become available, potentially delaying the necessary treatment. This delay underscores the importance of considering clinical symptoms and risk factors in conjunction with diagnostic tests for prompt and accurate diagnosis.
Imaging
Imaging plays a crucial role in diagnosing spinal tuberculosis, offering valuable insights into the extent and nature of the infection.
X-rays are often used initially and can reveal several characteristic signs of spinal tuberculosis, including decreased height of the vertebrae, bone erosion, rounding of the spine, and the presence of masses adjacent to the spine.
Magnetic resonance imaging (MRI) is particularly useful for visualizing soft tissues and can detect swelling in the bone marrow, abscesses within the bone, and narrowing of the spinal canal, which is the space surrounding the spinal cord. This imaging modality provides detailed information about the structural changes associated with spinal tuberculosis.
Computed tomography (CT scan) is another imaging technique that can offer detailed views of bone structures. It is especially helpful in assessing bone destruction caused by tuberculosis.
Positron emission tomography (PET scan) is employed to differentiate between bone infections and soft tissue infections. This imaging method aids in distinguishing areas of active infection from other types of tissue abnormalities.
By combining the information obtained from various imaging modalities, healthcare providers can make a more accurate diagnosis of spinal tuberculosis, enabling timely and appropriate treatment interventions.
Treatment
TTreatment for spinal tuberculosis typically involves a multifaceted approach that combines medications and other interventions tailored to the individual's condition and the severity of the damage caused by the infection.
Medications used in the four-month protocol include:
- Priftin (rifapentine)
- Avalox (moxifloxacin)
- Rifater, Rimstar, Voractiv (pyrazinamide)
- Hydra, Hyzyd, Isovit, (isoniazid)
Medications used in the six- or nine-month "RIPE" protocol include:
- Rifampin
- Isoniazid
- Pyrazinamide
- Ethambutol
Surgery
Surgery is frequently a necessary component of treatment for spinal tuberculosis, particularly when there is extensive damage to the bones and surrounding tissues. The specific surgical procedures employed depend on the severity and location of the bone damage.
- Debridement: This surgical procedure involves the removal of infected or necrotic (dead) tissue from the affected area. Debridement aims to eliminate the source of infection and promote healing.
- Bone Removal: In cases where the vertebrae have been significantly eroded by tuberculosis infection, surgical removal of the affected bone may be necessary to alleviate pressure on the spinal cord and nerves.
- Spinal Stabilization: Stabilizing the spine is crucial for maintaining proper alignment and preventing further damage. Surgeons may use screws, rods, plates, or other devices to stabilize the spine and maintain its integrity.
- Vertebral Fusion: Fusion surgery involves joining two or more vertebrae together to create a single, solid bone. This procedure helps stabilize the spine and may be necessary when there is extensive bone loss or instability.
- Bone Grafting: Bone grafting involves transplanting bone tissue from another part of the body, such as the hip or pelvis, and grafting it onto the spine. This helps promote bone growth and fusion, providing additional support to the spine.
Surgery for spinal tuberculosis is complex and carries inherent risks, including infection, bleeding, and nerve damage. However, it is often essential for relieving pain, stabilizing the spine, and preventing further neurological complications. Close collaboration between the patient, orthopedic surgeons, and other healthcare professionals is crucial to ensure the best possible outcomes from surgical intervention.



